Titanium is characterized by excellent corrosion behavior and thus has good immunological compatibility compared to other metals. However, both orthopedists and dentists know that in some patients, implants induce undesirable inflammatory symptoms that can lead to lack of bony integration, perigingivitis and periimplantitis.
True cellular type IV sensitization to titanium is a rarity. The reason is that ionic titanium in the medium pH range oxidizes immediately after release. In contrast to metal ions, oxidized titanium particles are not able to become allergens via modification of proteins. The frequently made statement that "there are no allergies to titanium" is therefore very probably correct from a strictly immunological point of view. However, allergies are not the only cause of immunologically induced intolerances. The most common cause of individual hypersensitivity to titanium is an excessive pro-inflammatory reactivity of tissue macrophages to titanium wear particles.
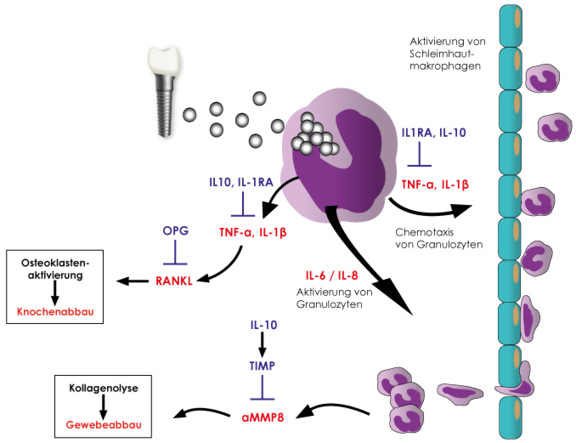
Metallic abrasion takes place on the surface of implanted titanium materials. These titanium oxide particles have a size between 1 and 10 µm and are almost always found in the surrounding bone or soft tissue of the implant. Tissue macrophages phagocytose the titanium oxide particles in the vicinity of titanium implants (particulate debris).
It is now known that the most common cause of individual hypersensitivity to titanium is an excessive pro-inflammatory reactivity of tissue macrophages to these debris particles.
It is physiological for macrophages to respond to contact with titanium oxide particles by releasing pro-inflammatory cytokines, essentially TNFα and interleukin-1. However, the extent of this immune response is very individual. The intensity of cytokine release depends on genetic variants (polymorphisms) of the pro-inflammatory (IL-1 and TNFα) and anti-inflammatory (IL-1 receptor antagonist IL-1RN) mediators involved. Titanium-specific lymphocytes, in contrast to all other metals, do not play a role here, which explains the negative LTT and epicutaneous test results.
For this question, the titanium stimulation test was developed and validated (Dörner T et al. 2006). This whole blood stimulation test examines whether the patient's monocytes/macrophages react with an increased inflammatory response after contact with titanium particles. This is recognizable by an increased release of the two key pro-inflammatory cytokines TNFα and/or IL1β. In patients with positive findings, delayed or impaired healing of titanium implants can be explained by the fact that the macrophages in the implantation area also react hyperactively to released titanium particles and primarily induce local inflammation.
The extent and course of the titanium-induced inflammatory response have been shown to be determined by the ratio of pro- and anti-inflammatory cytokines. The intensity with which the cytokines are released in the immune response is individually determined by functionally relevant polymorphisms in the cytokine genes. Meanwhile, for these polymorphisms in the genes of the cytokines IL-1, IL-1RN and TNF-α, the connection to peri-implantitis, implant loss and premature loss of marginal bone around endosseous dental implants has been shown in a large number of studies. The known polymorphisms in the TNF-α, IL-1, and IL1-RN genes can be detected in the laboratory. This molecular genetic procedure has the advantage of not being influenced by current inflammatory events or immunosuppressive therapies. Genetic testing allows assignment to a grade of inflammation based on the allele combination found. Patients with grade 3-4 are considered high-responders and thus at risk for titanium-associated inflammation/implant loss (see table below).
The early detection and evaluation of a predisposition to aseptic peri-implantitis, which can be associated with primary or secondary titanium implant loss, is of great importance, especially for preventive issues. In a study initiated by the German Society of Environmental Dentistry (DEGUZ), the prognostic significance of the titanium stimulation test and the genetic degree of inflammation was confirmed (Jacobi-Gresser et al. 2013). Compared to the control group (68 patients in whom implants have healed without problems for more than 5 years), patients with implant loss without loading during the healing phase (n = 14) as well as patients with implant loss after loading (n = 29) showed significantly higher in vitro titanium oxide-induced TNF-α and IL-1β release in the titanium stimulation test (p<0.0001). A positive titanium stimulation test represents a risk factor independent of age, gender, and smoking status, and increases the risk of titanium-associated inflammation/implant loss by 12-fold. In addition, the number of polymorphisms in the IL1, IL-1RN, and TNFa genes, and thus the resulting genetic degree of inflammation, has a significant impact on implant loss (p* = 0.046). As the degree of inflammation increases, the risk of titanium-associated inflammation/implant loss also increases.
Relative risk for titanium implant lost
| Grade 0 | 1,0 |
| Grade 1 | 1,5 |
| Grade 2 | 2,4 |
| Grade 3 | 3,8 |
| Grade 4 | 6,0 |
| Positive titanium stimulation test | 12,0 |
A positive titanium stimulation test (p<0.0001) and an increasing degree of inflammation (p<0.046) represent risk factors for titanium-associated inflammation/implant loss that are independent of gender, age, and smoking status and are therefore additive.
A conspicuous result in one of the two examinations indicates the presence of a predisposition to a titanium-associated inflammatory event, which may be associated with primary or secondary implant loss. It is not the same as an allergy, in which case the allergen should be avoided. In principle, the process of implant loss is a multifactorial event, which is why a positive titanium stimulation test and/or a highresponder gene constellation do not in themselves constitute an absolute contraindication for a titanium implant. However, the following should be considered for patients with positive constellations of findings:
- These affected patients have a significantly increased risk of titanium-associated inflammation or titanium implant loss. They do not have an allergy to titanium.
- In patients with an existing risk constellation, alternatives to titanium should be considered (zirconium dioxide implants, removable dentures, coated titanium implants).
- If, despite an existing risk constellation, a decision is nevertheless made in favor of titanium, the following can be considered, among other things:
- Intensified prophylaxis
- No use of periodontal probes made of titanium
- Implantation not in the pre-inflamed bone area
- intensive therapy of existing local inflammations ("foci") before and after implantation
- anti-inflammatory medication
- smoking cessation
- optimal control of other predisposing diseases (e.g. diabetes mellitus)
- In these patients, in addition to stimulus elimination, anti-inflammatory but never immunostimulatory therapy is more indicated.
By combining the two laboratory tests, early risk evaluation or diagnosis can be made, allowing either prior selection of alternative materials or early intervention to minimize tissue damage and increase the chances of success.
As already mentioned, type IV sensitization to titanium is extremely rare, which is due to the high oxidation tendency of titanium. However, depending on the implant system to be used, traces of nickel, vanadium or aluminum may be present. Therefore, additional testing for type IV sensitization to these metals may be required (LTT). Positive results would then also have to be taken into account when selecting the implant system.
- Titanium implants and silent inflammation in jawbone – a critical interplay of dissolved titanium particles and cytokines TNF-a and RANTES/CCL5 on overall health?
Johann Lechner J, Sammy Noumbissi, Volker von Baehr, EPMA Journal (2018). doi.org/10.1007/s13167-018-0138-6
Titanimplantate und stille Entzündungen im Kieferknochen - ein kritische Verbindung von gelösten Titanpartikeln und den Zytokinen TNF-a und RANTES / CCL5 mit systemischer Gesundheit?
Abstract: From a systemic perspective, we recommend that more attention be paid to cytokine overexpression caused by dissolved Ti particles from DTI in medicine and dentistry. - Prognose der Einheilquote von Titanimplantaten anhand von Laborparametern - eine retrospektive Studie
Dr. Elisabeth Jacobi-Gresser
- Titan als möglicher Verursacher lokaler und systemischer Gesundheitsstörungen - eine aktuelle praxisorientierte Zwischenbilanz
Dr. Frank Bartram